Healthcare Cost Assistance
Access the care you need to thrive.
Benefit Summary
Check out this overview video to learn about Healthcare Cost Assistance benefits.
Carewell SEIU 503 Healthcare Cost Assistance benefits help make individual health (medical) plans affordable for Oregon homecare and personal support workers who can’t get coverage through other means. Examples of other means include the Oregon Health Plan, another employer, or spousal coverage.
This benefit is available to eligible homecare and personal support workers who have Medicare or who enroll in an approved plan through a Health Insurance Marketplace. The Healthcare Cost Assistance benefit covers up to $7,165 of out-of-pocket medical expenses for claims covered by Medicare or your approved Marketplace plan in 2025. It also covers 100% of your net monthly premiums for your individual Marketplace plan, or a portion of your Medicare premiums.
If you’re eligible for Healthcare Cost Assistance, you receive a Benefit Convenience Card (a Mastercard credit card) to pay for your monthly premiums (unless you have Medicare) and covered out-of-pocket medical expenses. The card comes from Ameriflex (the Benefits Convenience Administrator).
Information for Healthcare Cost Assistance benefits for homecare and personal support workers
Important Things to Know
- This benefit pays your net monthly premium (your premium after tax credits have been applied) for a Carewell-approved individual plan purchased through the Marketplace or for Medicare. It also covers up to $7,165 in 2025 in out-of-pocket medical expenses for claims covered by your Carewell-approved individual plan or by Medicare. Carewell SEIU 503 Healthcare Cost Assistance benefits are not employer-sponsored or group coverage.
- To take advantage of this benefit, you need to enroll in a Carewell-approved plan on a Health Insurance Marketplace or in Medicare. Call us — 1-844-503-7348 — we’re here to help walk you through the process!
- In most cases, you need to wait until Open Enrollment to enroll. Open Enrollment on the federal Marketplace is generally between November 1 and December 15 for the following year. There are some exceptions that may qualify you to enroll through a Special Enrollment Period. See the Frequently Asked Questions for more information.
Eligibility
To find out your eligibility instantly, answer a few questions on the eligibility questionnaire.
Please read the eligibility requirements below carefully.
Eligibility Requirements
You are likely eligible for Healthcare Cost Assistance benefits if you:
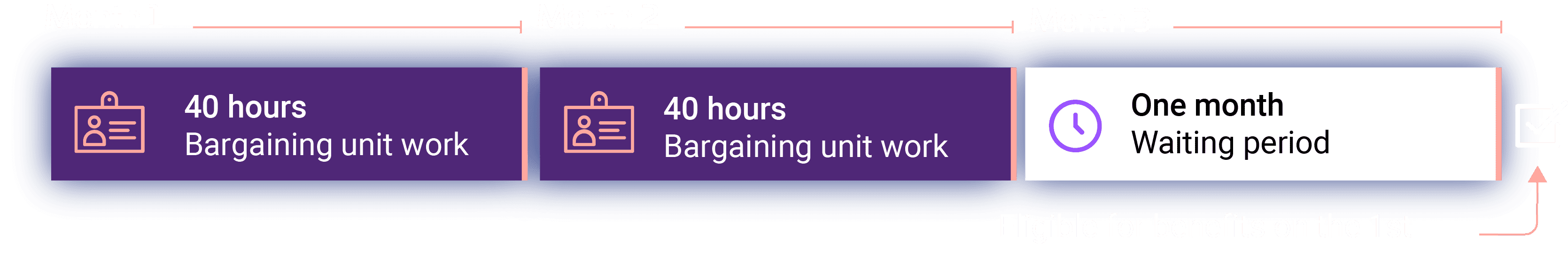
You worked at least 40 eligible working hours* for 2 months in a row. Once you meet this requirement, there is a 1-month waiting period after you turn in your timesheets and/or payroll vouchers. During this waiting period, the State, Acumen, or PPL will report your hours to Carewell SEIU 503.
Turn in your timesheets and/or payroll vouchers every pay period.
Have your name, gender, Social Security number, birth date, and current address on file with Carewell SEIU 503.
Have medical coverage through Medicare or through an approved Marketplace plan. See FAQs for more information.
These eligibility requirements are the same for the Dental, Vision + Hearing, and Employee Assistance Program (DVE) benefits.
* Eligible working hours
The number of eligible working hours you need to qualify for Carewell benefits are the work hours paid by Acumen, DHS, and/or PPL on behalf of your consumer.
Losing eligibility
You may lose eligibility for Carewell SEIU 503 Healthcare Cost Assistance benefits if you have 2 months in a row with 0 hours of work. After those 2 months, you’ll have a waiting period of 1 more month before your benefits end. You can regain eligibility for Carewell SEIU 503 benefits by meeting the requirements listed above. Eligibility rules are changing October 1, 2025. Learn more here.
Losing Carewell SEIU 503 benefits doesn’t mean you’re losing your health (medical) insurance coverage! But at the end of your waiting period month, your Benefit Convenience Card (BCC) is turned off and you have to start paying your own premiums and out-of-pocket medical expenses.
For eligible workers with Medicare
Learn more about Healthcare Cost Assistance for eligible workers covered by Medicare.
For eligible workers with approved plans
Learn more about Healthcare Cost Assistance for eligible workers with approved individual health (medical) plans on the Health Insurance Marketplaces.